ACUTE CORONARY SYNDROME
WHAT ARE ACUTE CORONARY SYNDROMES?
Acute coronary syndrome (ACS) is a term used to denote any condition that occurs as a result of reduced blood supply to the heart muscle. The disorders range from a threatened heart attack, also known as unstable angina, to an actual heart attack, called myocardial infarction.
ACS IS ALSO KNOWN AS:
- HEART ATTACK
- UNSTABLE ANGINA
- MYOCARDIAL INFARCTION
WHAT CAUSES ACUTE CORONARY SYNDROME?
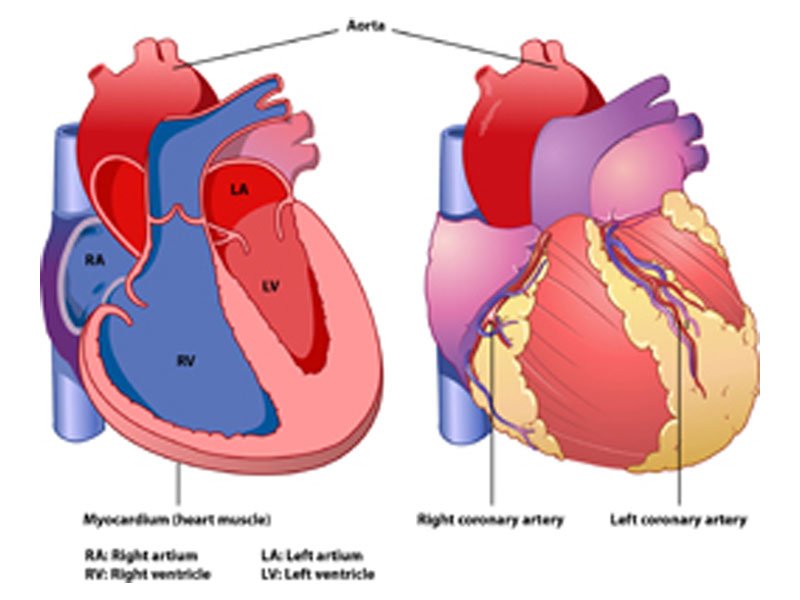
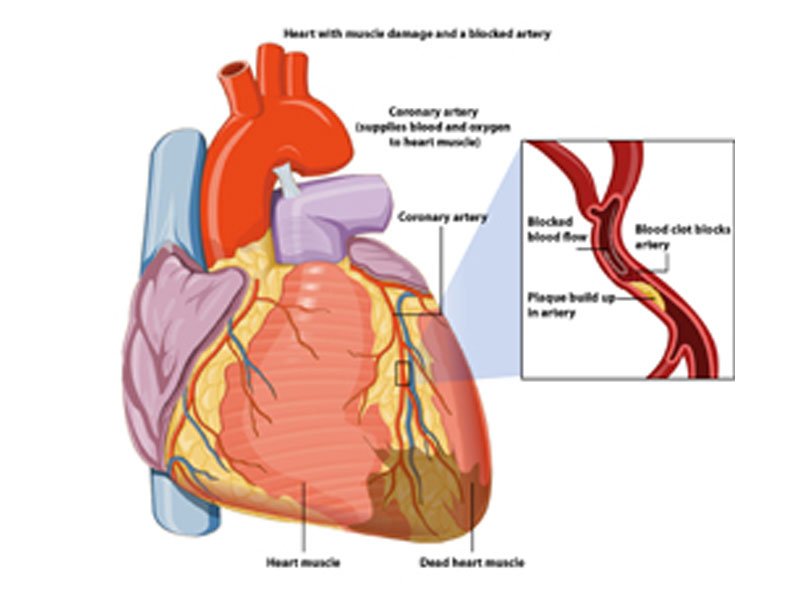
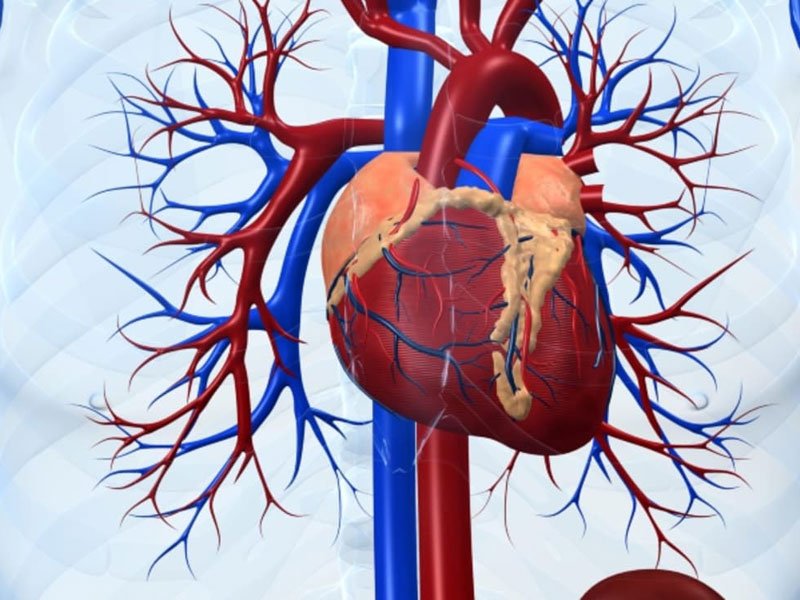
The blood vessels that carry blood away from the heart are known as arteries. The heart supplies oxygen-rich blood to the various parts of the body through an artery called aorta. The coronary arteries that branch off from the aorta in turn carry blood to the heart muscle. Any factor that reduces the blood flow to the heart muscle, either due to blood vessel narrowing or blockage, can lead to ACS. One of the most common causes of blood vessel narrowing is atheroma formation. Atheroma refers to deposits called plaques that develop in the wall of the arteries overtime. The plaques comprise an outer hard shell with an inner fatty core. These can impede the blood flow to the heart by narrowing the arterial lumen, that is, the cavity of the arteries. Apart from atheroma, inflammation of the coronary arteries, stab wound to the heart, cocaine abuse, migrating blood clot and surgical complications are a few other conditions causing vessel blockage. Figure 1 illustrates the chambers and different arteries supplying blood to the heart.
WHAT IS MEANT BY UNSTABLE ANGINA AND MYOCARDIAL INFARCTION?
Unstable angina
Myocardial infarction

WHAT ARE THE SIGNS AND SYMPTOMS OF ACUTE CORONARY SYNDROME?
The symptoms of ACS are similar to that of a heart attack, and if unattended instantly, it can lead to an actual attack. Signs and symptoms of ACS include:
- Sudden discomfort in the chest, which can be burning, squeezing or painful in nature
- Discomfort or pain radiating to the jaw, shoulder or arm
- Nausea and/or vomiting
- Increased sweating
- Shortness of breath (dyspnoea)
Atypical symptoms include:
- Feeling of heartburn
- Pain in the abdomen
- Severe fatigue and restlessness
WHAT SHOULD BE DONE IN CASE OF A HEART ATTACK?
When in doubt of having a heart attack, urgent medical help should be sought. An early intervention can prevent severe damage. Driving on own should be discouraged. An ambulance can be called for further assistance.
WHAT IS CARDIOPULMONARY RESUSCITATION AND HOW SHOULD IT BE PERFORMED?
Brain damage can occur secondary to lack of oxygen-rich blood after the heart stops working. To restore the blood circulation, cardiopulmonary resuscitation (CPR) can be very useful. CPR is a procedure for maintaining the functioning of the heart and restoring the breathing function of the lungs.
The American Heart Association recommends the following while performing a CPR:
- If you are not trained in CPR, then provide about 100 chest compressions per minute until the arrival of paramedics
- If you are trained in CPR and confident, begin with 30 chest compressions before checking the airways and initiating rescue breaths
- If you are trained and not confident enough, provide about 100 chest compressions per minute until the arrival of paramedics
Another form of resuscitation that is gaining popularity is cardiocerebral resuscitation, in which recommends on continuous chest compressions without mouth-to-mouth breathing.
WHO IS AT RISK OF HAVING A HEART ATTACK?
Risk factors of a heart attack are similar to that of any other heart disease. These are classified into modifiable and non-modifiable risk factors. Modifiable risk factors include:
- Smoking
- Hypertension
- Obesity
- High cholesterol
- Lack of physical activity
Non-modifiable risk factors include:
- Age (over 45 years for men and 55 for women)
- A family history of heart disease
- Preeclampsia (pregnancy-induced hypertension)
HOW IS ACUTE CORONARY SYNDROME DIAGNOSED?
It is important to differentiate the pain caused by ACS from the pain due to other causes. Various tests that help in appropriate diagnosis have been discussed below:
ELECTROCARDIOGRAM (ECG/EKG)
BLOOD SAMPLE
ECHOCARDIOGRAM
CHEST X-RAY
NUCLEAR SCAN
COMPUTERISED TOMOGRAPHY (CT) ANGIOGRAM
ANGIOGRAPHY (CORONARY ANGIOGRAM/ CARDIAC CATHETERISATION)
HOW IS ACUTE CORONARY SYNDROME TREATED?
TREATMENT IN THE FIRST 12 HOURS
MEDICAL MANAGEMENT
BLOOD THINNING TREATMENT
Aspirin and clopidogrel A combination of aspirin and clopidogrel is recommended in patients with:
- Change in rhythm of the heart
- Raised cardiac enzymes (troponin) levels
Glycoprotein llb/lla receptor antagonist Patients who are at increased risk of having a heart attack or undergoing a procedure called angioplasty (percutaneous coronary intervention)are usually prescribed glycoprotein llb/lla receptor antagonist. These drugs are given intravenously (directly inside the veins),which helps in widening the blocked arteries.
ANTICOAGULANTS
BETA BLOCKERS
CARDIAC MONITORING
INSULIN THERAPY
INVASIVE MANAGEMENT
ANGIOGRAPHY AND REVASCULARISATION
Patients in whom invasive procedures are considered include:
- Patients with non-ST elevation acute coronary syndromes at medium to high risk of early recurrent cardiovascular events
- Patients with ST elevation acute coronary syndromes treated with thrombolytic therapy
After the first 12 hours have passed, the coronary arteries are unblocked using coronary angiography and revascularisation. The range of procedures that aid in unblocking a narrowed artery is termed as revascularisation.
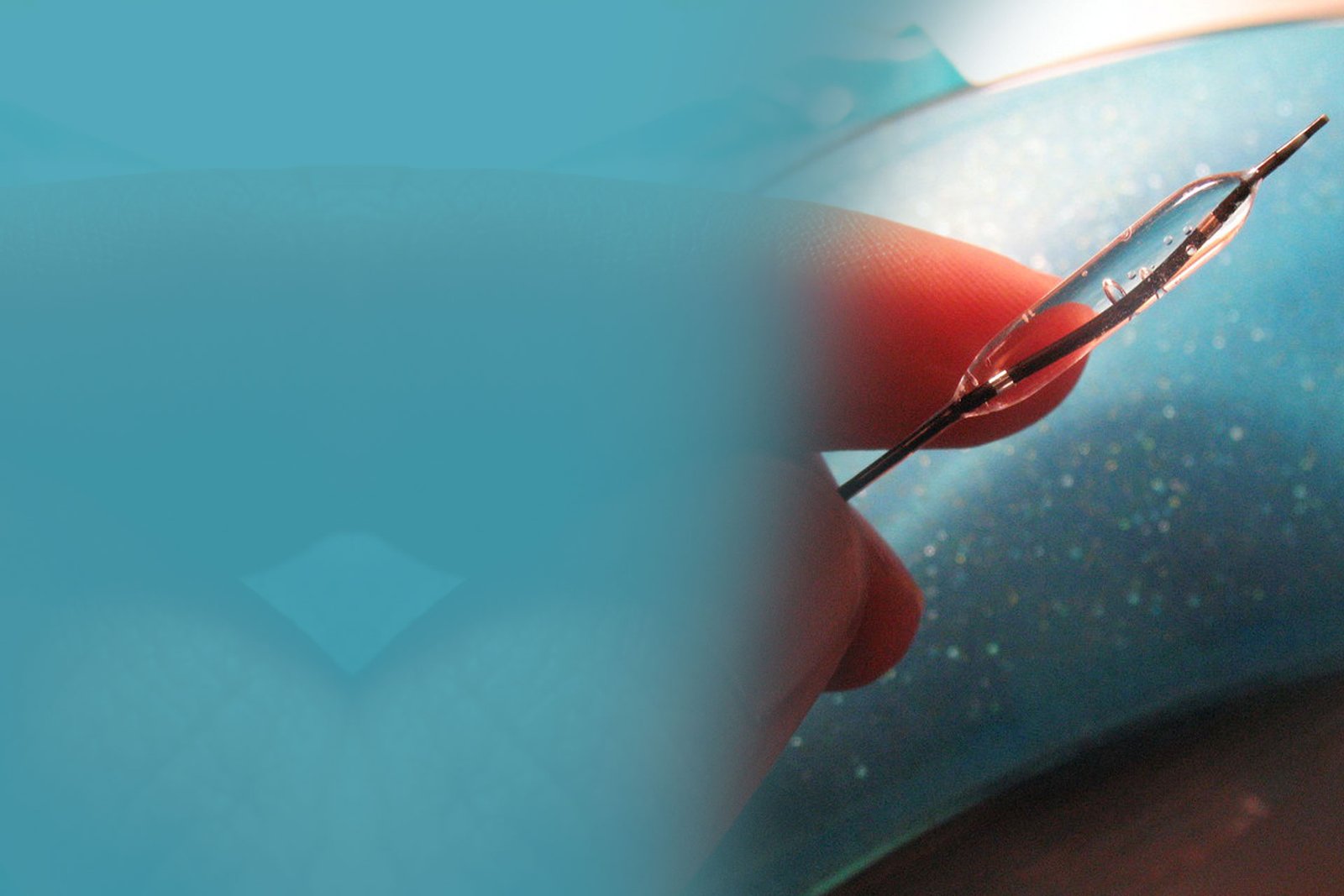
PRIMARY ANGIOPLASTY (PRIMARY PERCUTANEOUS CORONARY INTERVENTION)
This procedure is basically performed to widen a blocked or narrowed artery. A small tube called catheter with a deflated balloon at its tip is inserted in to the coronary artery via an artery in the groin or arm. X-rays are used to gain access to the coronary artery and the blocked area within. Upon reaching the narrowed segment, the balloon is inflated, which compresses the fatty deposits, thereby widening the artery. A small steel mesh, called stent, is left in place to keep the artery open. Glycoprotein llb/lla receptor antagonists are administered along with the procedure to reduce pain and decrease the formation of clots.
RESCUE ANGIOPLASTY (RESCUE PERCUTANEOUS CORONARY INTERVENTION)
In a patient presenting with acute coronary syndrome, if thrombolytic therapy fails to reperfuse the infarcted myocardium within 6 hours of symptom onset, a rescue angioplasty is performed.
BYPASS HEART SURGERY (CORONARY ARTERY BYPASS GRAFT/CABG)
Bypass heart surgery is an alternative surgical procedure to treat a heart attack. It involves grafting or connecting a healthy vessel (artery or vein) to the blocked coronary artery to bypass the blockade, hence, providing an alternative route for blood to go around a blocked coronary artery.
THROMBOLYTIC THERAPY
Thrombolytics
Also known as ‘clot busters’, thrombolytics are the drugs that help in dissolving clots and clearing the block. Thrombolytics need to be administered as soon as possible if angioplasty is not performed in the first 90 minutes after diagnosis; early treatment minimises the damage to the heart muscle and improves survival rates.
TREATMENT BEYOND THE FIRST 12 HOURS
SURGICAL MANAGEMENT
Cardiac surgery
Patients presenting with rupture of cardiac muscle in heart attack should undergo corrective surgery within 24 to 48 hours.
WHAT ARE THE COMMON MEDICINES PRESCRIBED AFTER A HEART ATTACK?
ANGIOTENSIN-CONVERTING ENZYME (ACE) INHIBITORS AND ANGIOTENSIN RECEPTOR BLOCKERS (ARBS)
- Heart attack
- Unstable angina or
- Heart tissue damage
ANTIPLATELETS
- Patients with unstable angina scheduled for an invasive procedure
- Patients with drug-eluting stents to prevent the formation of clots
- Patients with heart attack undergoing angioplasty (percutaneous coronary intervention) or thrombolytic therapy
BETA BLOCKERS AND ANTI-ANGINAL THERAPY
EPLERENONE
CHOLESTEROL-LOWERING DRUGS
CARDIAC REHABILITATION
- Exercise
- Education
- Counselling
- Training to prevent a future episode of ACS
EPLERENONE
CHOLESTEROL-LOWERING DRUGS
WHAT ARE THE COMPLICATIONS ASSOCIATED WITH ACS?
Complications of ACS include:
- Pulmonary oedema: Fluid collection in the lungs leading to dyspnoea (shortness of breath)
- Cardiogenic shock: A sudden drop in the blood pressure along with reduced blood flow
- Heart muscle rupture
- Long-lasting pain
HOW CAN YOU PREVENT ACS?
ACS can be prevented by adopting a heart healthy lifestyle.
QUIT SMOKING
Smoking can adversely affect the heart and blood vessels. Smoking is an independent risk factor for the development of heart disease. Smoking damages the function of the heart and blood vessels and accelerates the progression of atherosclerosis (a condition where a deposit called plaque blocks the arteries and causes narrowing of the arterial cavity). Passive or second-hand smoking can also be detrimental for the health of the arteries and the heart and can increase the risk of heart attack substantially.
Quitting smoking at any age has huge health benefits. People who quit before the age of 50 or after 60 have decreased risk of cardiovascular events.
FOLLOW A HEALTHY DIET
Patients at risk of ACS and those after an episode of ACS are advised to restrict their salt and fat intake. This helps in keeping the blood pressure and cholesterol in control. A wholesome, low-fat diet that includes fruits, vegetables and grains is recommended.
CONTROL BODY WEIGHT
Obesity is a risk factor for coronary heart disease and heart attack. Moderate exercise for around 30 minutes a day can promote weight loss and help in controlling the levels of sugar, cholesterol and blood pressure. Regular exercise also helps in improving the blood flow to the heart and increases stamina. However, it is advisable to consult a doctor before initiating any exercise programme.
PERIODIC BLOOD TESTS TO ASSESS CHOLESTEROL LEVELS
Cholesterol levels need to be checked at frequent intervals. The recommended lipid levels are:
| Total cholesterol | <200 mg/dL |
|---|---|
| Low-density lipoprotein cholesterol | <130 mg/dL for individuals at low risk <100 mg/dL in people with moderate risk <70 mg/dL for those with high risk |
| High-density lipoprotein cholesterol | >40 mg/dL for men >50 mg/dL for women |
Diet changes and medications are prescribed in case of increased lipid levels.
MAINTAIN NORMAL BLOOD PRESSURE
Blood pressure should be checked every 2 years and more frequently if already on treatment for hypertension and/or heart disease. The normal blood pressure is <120/80 (systolic/diastolic) millimetres of mercury (mm Hg).
MANAGE STRESS LEVELS
Reduction of stress levels decreases the risk of heart attack in individuals. Lifestyle changes should be considered to manage stress levels efficiently.
MODERATE CONSUMPTION OF ALCOHOL
Alcohol should be consumed in moderation as excessive drinking can increase the blood pressure.
HOW IS LIFE AFTER AN EPISODE OF ACS?
- Patients after an attack can have a better quality of life if prompt treatment is administered
- Earlier the treatment better is the chances of recovery
- Regular follow-ups with the doctor are essential
- Patients who do not have chest pain can resume normal daily activities within a few weeks
- If the condition is associated with complications, patients should refrain from driving till the symptoms are stabilised
- Professional counselling and health groups can help in coping with post-attack anxiety; medications can be prescribed if required

