CORONARY
WHAT ARE ACUTE CORONARY SYNDROMES?
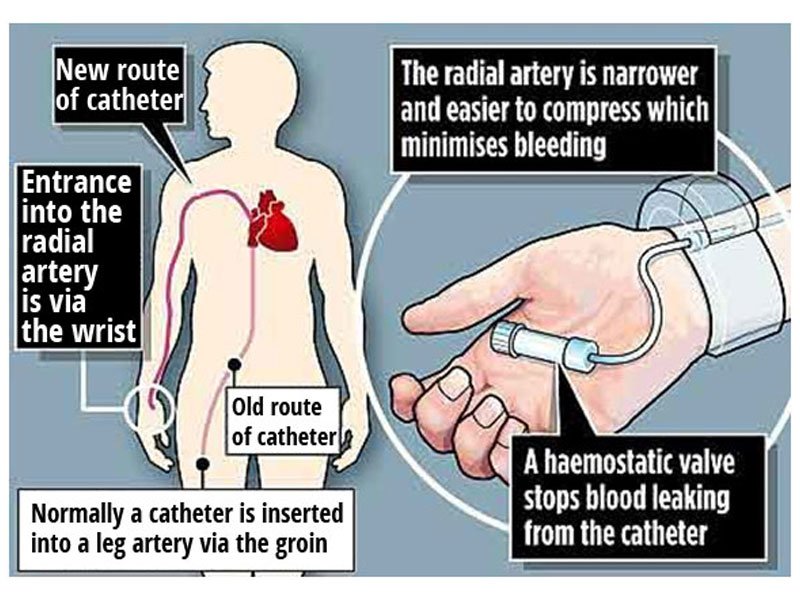
Interventional Cardiology is a subspecialty of cardiology in which catheter-based diagnostic tests and treatment are provided for coronary artery disease, valvular disease, structural heart disease, peripheral vascular disease and various other diseases. Interventional cardiology is a branch of cardiology that deals specifically with the catheter based treatment of structural heart diseases.
A large number of procedures can be performed on the heart by catheterization. This most commonly involves the insertion of a sheath into the femoral artery (but, in practice, any large peripheral artery or vein) and cannulating the heart under X-ray visualization (most commonly fluoroscopy). The radial artery may also be used for cannulation; this approach offers several advantages:
1. Easy accessibility of the artery in most patients,
2. Easy control of bleeding even in anticoagulated patients,
3. More comfortable to the patient because they are capable of sitting up and walking immediately following the procedure, and
4. The near absence of clinically significant sequelae in patients with a normal Allen test.
The main advantages of using the interventional cardiology or radiology approach are the avoidance of the scars and pain, and long post-operative recovery. Additionally, interventional cardiology procedure of primary angioplasty is now the gold standard of care for an acute myocardial infarction.

Interventional Cardiology procedures can include:
- Balloon Angioplasty creates a space in a blocked artery by inserting and inflating a tiny balloon. The balloon compresses the plaque against the wall of the artery so blood can flow more freely. The balloon does not remain in the body.
- Intracoronary Stenting requires the permanent insertion of a tiny stainless steel wire-mesh tube called a stent to keep arteries open following a balloon angioplasty. Both bare-metal and drug-eluting (medication-releasing) stents are available.
- Carotid Stents and Stroke Intervention involves the insertion of a stent to expand the carotid arteries located on each side of the neck, extending from the aorta to the base of the skull to supply blood to the brain. If a clot or plaque blocks the blood flow to the brain, it can cause a stroke, resulting in brain damage or death.
- Congenital Heart Defect Correction can be employed to correct atrial septal and ventricular septal defects, closure of a patent ductus arteriosus and angioplasty of the great vessels.
- Fractional Flow Reserve (FFR) can accurately measure blood pressure and flow through a specific part of the coronary artery. The measurement of FFR has been shown useful in assessing whether or not to perform angioplasty or stenting on intermediate blockages.
- Intravascular Ultrasound involves a small catheter in the coronary artery to emit sound waves that produce an image of the blockage, providing the cardiologist with needed information to best manage the blockage.
- Implantable Cardioverter Defibrillators (ICDs) help treat patients at high risk for sudden cardiac arrest. Implanted through a small incision near the shoulder, ICDs use electrical pulses or shocks to help control life-threatening and irregular heartbeats.
- Pacemaker Insertion is for patients with abnormally slow heart rhythms, congestive heart failure and those at risk for sudden death. Pacemakers help coordinate the pumping action of the heart by sending electrical signals, allowing the heart to pump more effectively.
- Peripheral Arterial Disease (PAD) Intervention involves the evaluation of diseases of the blood vessels outside the heart. Balloon angioplasty and stenting may be used similarly to heart procedures to treat PAD.
- Peripheral Atherectomy cuts through plaque in the blood vessels outside the heart. The plaque is reduced to particles smaller than red blood cells, resulting in a smoother inner surface of the vessel that allows for increased blood flow.

